Back Burning Sensation Symptom Checker
Check Your Symptoms
Select any symptoms you're experiencing. This tool helps identify urgent red flags requiring immediate medical attention.
Ever felt a sudden, uncomfortable heat spreading across your back, as if a tiny fire had ignited under your skin? That burning sensation back can be alarming, but you don’t have to panic. Below you’ll learn what typically sparks this feeling, how doctors figure out the root problem, and which treatments actually work.
Quick Takeaways
- Burning back pain most often stems from nerve irritation, muscle strain, or spinal disc issues.
- Key red‑flags include numbness, weakness, fever, or a rash-see a clinician right away.
- Diagnosis usually combines a physical exam with imaging (X‑ray, MRI) and sometimes blood tests.
- First‑line treatments are rest, targeted stretches, and over‑the‑counter pain relievers.
- Persistent symptoms may need physical therapy, prescription medication, or minimally invasive procedures.
What Exactly Is a Burning Sensation in the Back?
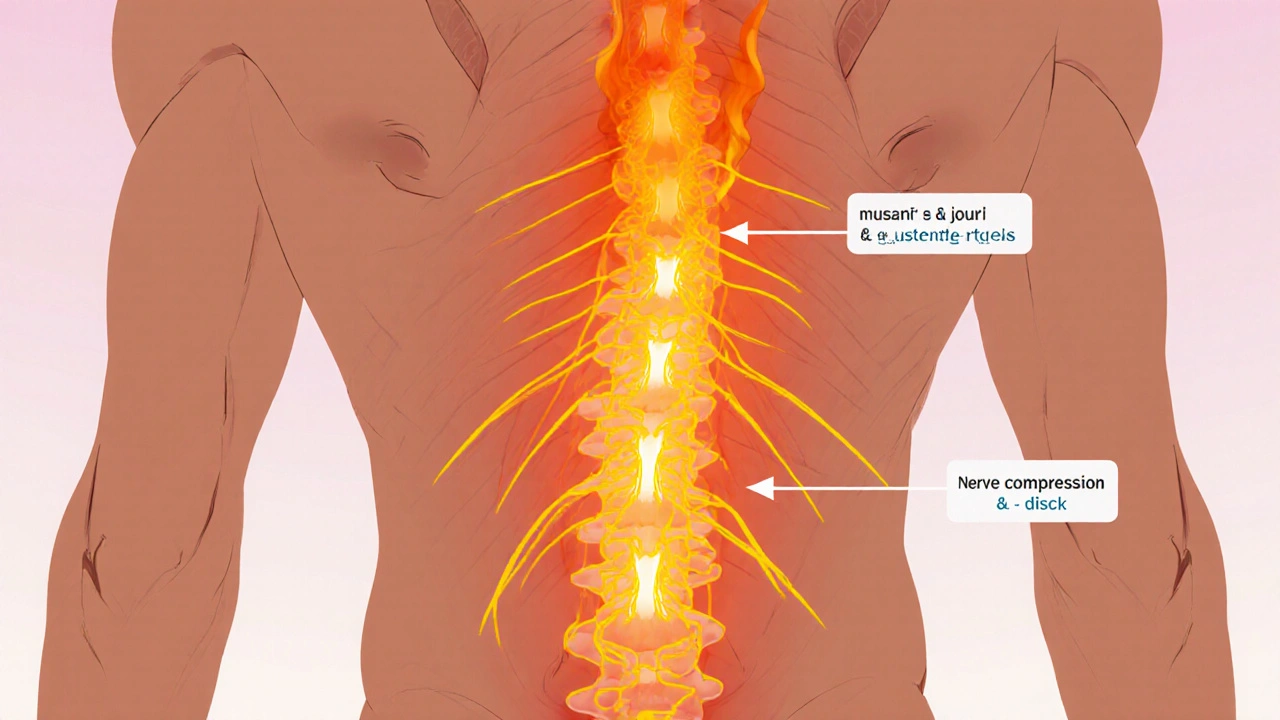
Burning sensation in the back is an uncomfortable feeling that feels hot, tingling, or like a mild electric shock, usually localized to the thoracic or lumbar region. It differs from a dull ache because it often involves the skin’s surface and can travel along a nerve pathway.
The sensation can be fleeting (minutes) or chronic (weeks to months). Understanding whether it’s skin‑deep or rooted in deeper structures is the first clue to treatment.
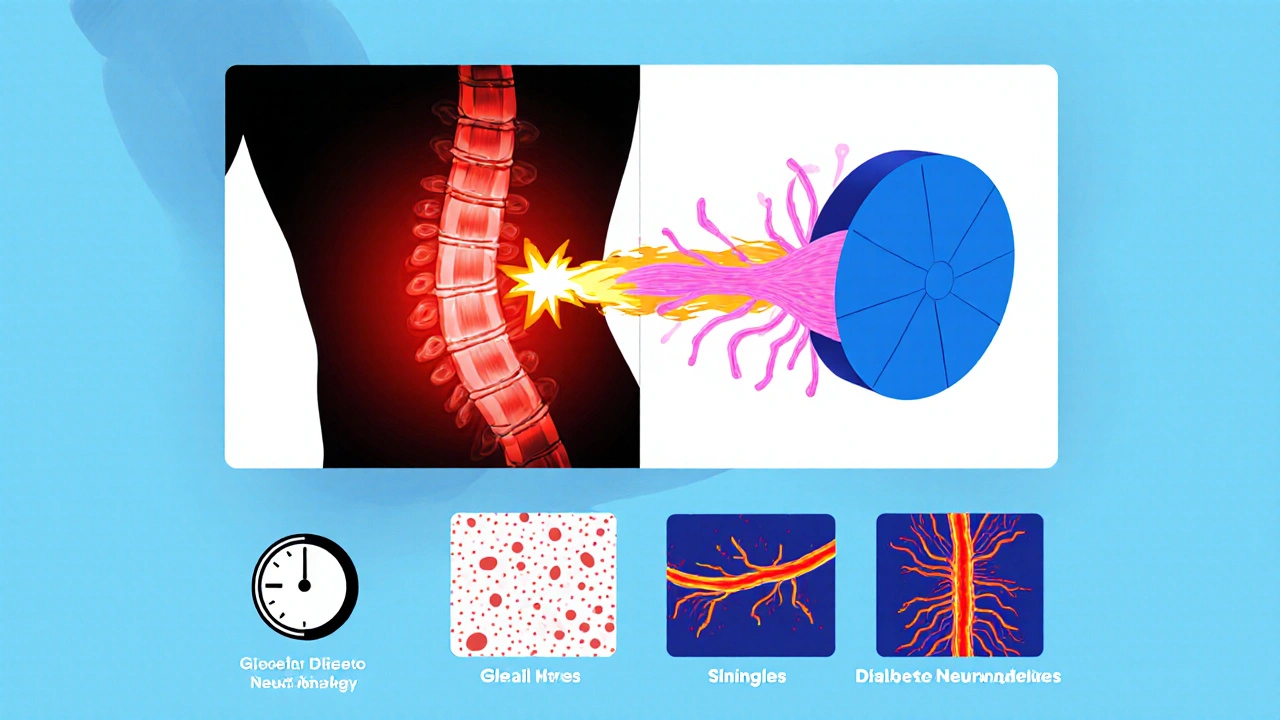
Common Causes - From Simple Strain to Nerve Problems
Below is a snapshot of the most frequent culprits. Each cause has its own pattern, triggers, and typical treatment route.
| Cause | Typical Symptoms | Common Triggers | First‑Line Test | Usual Treatment |
|---|---|---|---|---|
| Muscle strain | Localized heat, soreness, worsens with movement | Heavy lifting, sudden twist, poor posture | Physical exam, tenderness map | Rest, ice/heat, gentle stretching |
| Nerve compression (e.g., radiculopathy) | Burning that radiates down arm or leg, possible numbness | Disc bulge, spinal stenosis, prolonged sitting | Neurological exam, MRI | Physical therapy, NSAIDs, epidural steroid injection |
| Spinal disc herniation | Sharp burning, worsens with coughing or bending | Degeneration, trauma | MRI, CT scan | Core strengthening, traction, surgery if severe |
| Diabetic neuropathy | Persistent burning, often bilateral, tingling | Long‑standing high blood sugar | Blood glucose test, nerve conduction studies | Glycemic control, duloxetine, gabapentin |
| Shingles (herpes zoster) | Burning with a rash, usually one side of the torso | Reactivation of chicken‑pox virus | Clinical exam, PCR if unclear | Antiviral medication, pain control |
Red‑Flag Symptoms - When to Seek Immediate Care
Most back burning sensations are benign, but certain signs suggest a more serious condition. If you notice any of the following, call a healthcare professional right away:
- Sudden loss of strength or sensation in the legs
- Unexplained fever or chills
- Rash that follows a nerve line (possible shingles)
- Difficulty controlling bladder or bowels
- Severe, unrelenting pain that doesn’t improve with rest
How Doctors Diagnose the Underlying Issue
The diagnostic pathway starts with a detailed history and physical exam. Your clinician will ask when the burning began, what makes it better or worse, and whether you have other health conditions (diabetes, recent infections, etc.).
Key examination steps include:
- Palpation of the spine and surrounding muscles to locate tenderness.
- Neurological testing - checking reflexes, sensation, and muscle strength.
- Range‑of‑motion assessment - noting positions that trigger the burn.
If the exam points to nerve involvement or disc pathology, imaging is the next step. X‑rays show bone alignment, while MRI gives a clear view of soft tissues, discs, and nerves. In cases where infection or systemic disease is suspected, blood work (CBC, CRP, HbA1c) may be ordered.
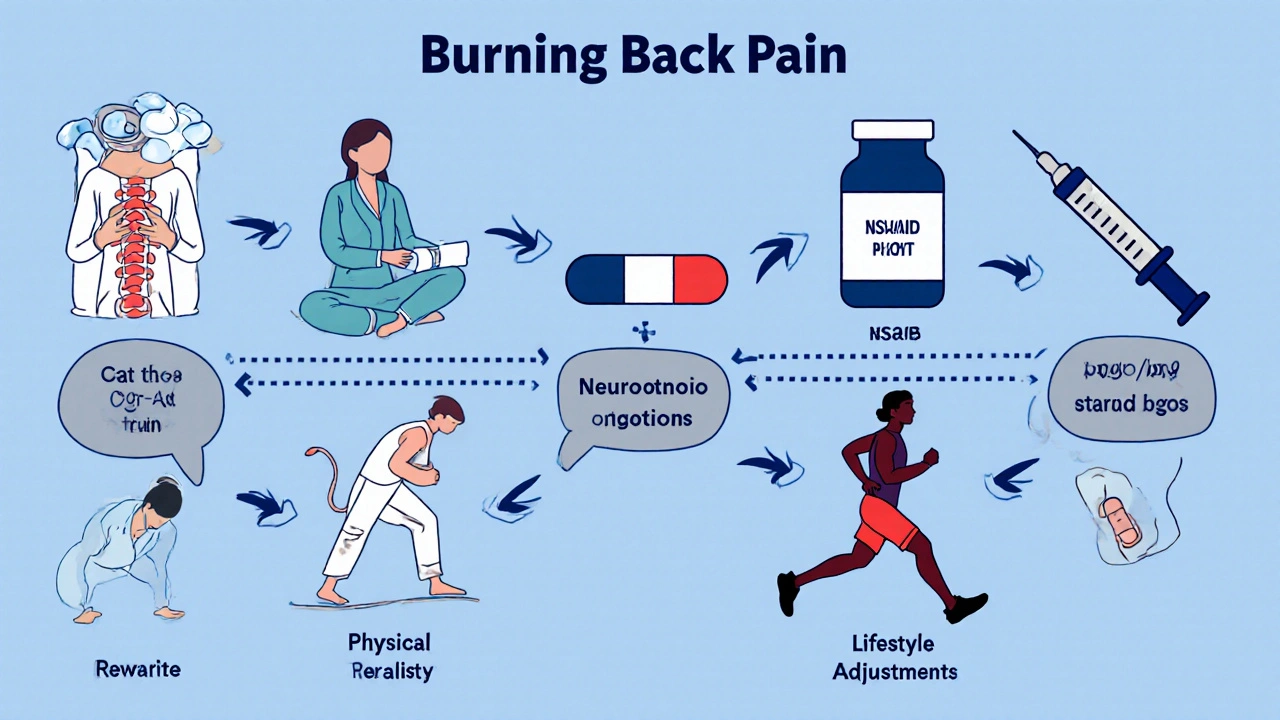
Treatment Options - From Home Care to Specialized Interventions
Management depends on the cause, severity, and your personal health profile. Below you’ll find the most common tiers of treatment.
1. Self‑Care Measures (First Week)
- Heat or cold therapy: Apply a cold pack for the first 48hours to reduce inflammation, then switch to a warm compress to relax muscles.
- Gentle stretching: Cat‑cow, child's pose, and seated thoracic rotations help alleviate muscle tension without over‑stretching nerves.
- Over‑the‑counter pain relievers: Ibuprofen (200‑400mg every 6‑8hours) or acetaminophen can lessen pain and swelling.
- Posture correction: Use lumbar support when sitting, keep screens at eye level, and avoid slouching for prolonged periods.
2. Physical Therapy (Weeks 2‑6)
Physical therapy is often the turning point for nerve‑related burning. A therapist will guide you through:
- Core‑strengthening exercises (planks, bird‑dog) that stabilize the spine.
- Neural glides that gently mobilize the affected nerve pathways.
- Manual therapy - soft‑tissue massage and joint mobilization to reduce compression.
Most patients report a noticeable drop in burning intensity after 4-6 sessions.
3. Prescription Medications (If OTC Fails)
When pain persists, doctors may prescribe:
- Neuropathic agents: Gabapentin 300mg at bedtime or duloxetine 30mg daily target nerve pain.
- Muscle relaxants: Cyclobenzaprine short‑term can ease spasms that exacerbate burning.
- Topical options: Capsaicin 0.075% cream applied 3‑4 times daily desensitizes nerve endings.
Always discuss side‑effects and interactions with your pharmacist.
4. Interventional Procedures (Severe or Chronic Cases)
For stubborn nerve compression, specialists may perform:
- Epidural steroid injection: Corticosteroid delivered near the irritated nerve reduces inflammation for weeks to months.
- Radiofrequency ablation: Heat‑generated lesion disables pain‑conducting fibers.
- Surgical decompression: Discectomy or laminectomy removes the offending disc material or bone spurs.
These options are usually considered after 3‑6 months of conservative care.
5. Lifestyle Adjustments for Long‑Term Relief
- Regular aerobic activity: Walking, swimming, or cycling improves blood flow to spinal tissues.
- Weight management: Excess weight adds load to the lumbar spine, increasing compression risk.
- Blood sugar control: For diabetic neuropathy, maintaining HbA1c below 7% slows nerve damage.
- Vaccination: The shingles vaccine (Shingrix) dramatically reduces the chance of a painful outbreak.
Preventing Future Episodes
Most burning sensations are preventable with simple habits:
- Start each day with a brief mobility routine - shoulder rolls, thoracic extensions, and hip hinges.
- Keep workstations ergonomically friendly: monitor at eye level, keyboard at elbow height.
- Lift with your legs, not your back; avoid twisting while lifting heavy objects.
- Stay hydrated - intervertebral discs rely on fluid to cushion nerves.
- Schedule regular check‑ups if you have chronic conditions like diabetes or rheumatoid arthritis.
Mini‑FAQ
Frequently Asked Questions
Can a burning sensation in the back be a sign of a heart attack?
Usually not. A heart attack typically causes pressure or squeezing in the chest that may radiate to the left arm or jaw. If you have chest pain, shortness of breath, or sweating, seek emergency care.
Why does heat sometimes make the burning feel worse?
Heat increases blood flow, which can amplify inflammation if the underlying issue is an acute nerve irritation. Use cold during the first 48hours, then switch to gentle warmth for muscle relaxation.
Is it safe to take ibuprofen if I have a stomach ulcer?
No. Ibuprofen can irritate the stomach lining. Talk to your doctor about alternatives like acetaminophen or a prescription COX‑2 inhibitor that’s gentler on the gut.
How long does it take for shingles‑related burning to subside?
With antiviral treatment started within 72hours, the rash and burning usually improve within 2‑3 weeks. Pain can linger for months (post‑herpetic neuralgia), so early therapy is key.
Can I continue exercising if I have a burning back sensation?
Low‑impact activities like walking or swimming are generally safe and may help. Avoid heavy lifting or high‑impact sports until the pain subsides. If burning worsens during exercise, stop and consult a therapist.
Next Steps - What to Do Right Now
If you’re reading this because the fire’s already lit, follow this quick roadmap:
- Assess red‑flags: Fever, rash, weakness → call your doctor or emergency services.
- Start self‑care: 20minutes of ice, then gentle stretches for the next 2‑3 days.
- Schedule an appointment: A primary care physician can order imaging if needed.
- Consider physical therapy: Book a session within a week if pain lingers beyond 5‑7 days.
- Track progress: Keep a simple log of pain intensity (0‑10) and activities that help or hurt.
Following this plan gives you the best chance to douse the burn before it becomes chronic.
Bottom Line
Burning sensations in the back are rarely a sign of a life‑threatening emergency, but they do signal that something in your musculoskeletal or nervous system needs attention. By spotting red‑flags, getting an accurate diagnosis, and applying a tiered treatment approach-from home care to specialist interventions-you can relieve the heat and get back to your daily routine.


Comments
First, congratulations on taking the time to understand what that fiery back feeling means – that’s half the battle won.
When you notice a burning sensation, the brain immediately sends a signal that something in your musculoskeletal or nervous system is irritated, and that’s a cue to act before things get worse.
Start by pausing any heavy activity; give the tissues a chance to settle down and avoid aggravating the inflammation.
Apply a cold pack for the first 48 hours; the cold constricts blood vessels, limits swelling, and can mute that uncomfortable heat.
After the initial chill, switch to a gentle warm compress; warmth promotes blood flow, helps muscles relax, and prepares the area for gentle movement.
Next, incorporate a short series of mobility drills – think cat‑cow, thoracic rotations, and seated side bends – each performed slowly for about ten seconds, three times a day.
Remember not to force any stretch; the goal is to ease tension, not to create a new strain.
Hydration plays a surprisingly big role – intervertebral discs are water‑rich and stay pliable when you drink enough fluids.
Keep a simple pain‑log, rating the burn on a 0‑10 scale before and after each activity; this will help you spot patterns and discuss them with a clinician.
If the burning spreads down a leg or arm, or you notice numbness, that’s a red flag pointing toward nerve compression, and you should schedule a visit with a physical therapist or spine specialist promptly.
For many people, over‑the‑counter NSAIDs like ibuprofen can reduce inflammation, but be mindful of gastrointestinal side effects if you have a history of ulcers.
Should NSAIDs be off‑limits, acetaminophen is a safer alternative for pain relief, though it won’t address inflammation directly.
When the acute phase settles, transition to core‑strengthening exercises – planks, bird‑dog, and gentle dead‑bugs – to build a supportive muscular wall around the spine.
These exercises not only stabilize the vertebrae but also take pressure off the intervertebral discs, which can prevent future burning episodes.
Finally, consider a short course of professional physical therapy; a trained therapist can tailor neural glides and manual techniques to your specific pattern of pain, often delivering noticeable relief within four to six sessions.
Stick to this roadmap, stay consistent, and you’ll likely douse that back‑fire before it becomes a chronic blaze.
The piece exaggerates disc problems while ignoring simple posture fixes.
One might contemplate the burning back as a metaphor for hidden stresses that surface when neglected.
In the quiet moments, the nervous system whispers about imbalance, urging us to realign both body and mind.
Observing the pattern of pain can reveal deeper habits, such as prolonged sitting or emotional tension.
Thus, treatment is not merely mechanical but also a call to introspection.
Gentle movement becomes a meditation, and each stretch a line of poetry written upon the spine.
By honoring the signal, we transform discomfort into insight and perhaps prevent future flare‑ups.
OMG this burning back feels like a tiny dragon just set my spine on fire! 🔥🔥 I was legit panicking, thinking I’d need surgery ASAP! 😱 But the tips in this post are like my superhero cape – saving the day! 🦸♀️💪 Seriously, apply ice, stretch, and watch the dragon chill out. 🙌✨
Listen up, comrades of the back! The fiery sting you feel is just a battle cry from your muscles demanding respect. ⚔️💥 Dive into the icy abyss for two days, then let the warm sun melt the tension – it’s a warrior’s routine! 🎯💪 Pump up your palate with vibrant veggies, stay hydrated like a waterfall, and let your core become a steel fortress. 🌈🏋️♂️ If the pain dares to linger, charge forward to a physio and smack that nerve compression into oblivion! Victory is yours, just keep the fire under control and the glory will follow.
Great rundown! 😊
While the guide suggests universal solutions, it overlooks how cultural work habits shape back pain; in many regions heavy manual labor is the norm and the advice must be tailored accordingly.
Indeed, the dramatization of a spinal “dragon” may capture attention, yet the clinical reality demands measured intervention rather than theatrical flair. A disciplined application of cryotherapy followed by structured physiotherapy remains the cornerstone of effective management, regardless of the narrative employed.
Your comprehensive roadmap is spot‑on; adhering to a pain log and progressive core work often yields measurable improvement within weeks.
It is commendable to adopt an enthusiastic tone; however, one must also underscore the importance of evidence‑based practice, particularly the judicious use of pharmacologic agents and the timing of interventional procedures as delineated in current clinical guidelines.
Interesting point! 😊 It’s true that posture plays a huge role, and simple desk adjustments can make a world of difference.