Almost everyone takes medication at some point - whether it’s a daily pill for blood pressure, an antibiotic for an infection, or a painkiller after a workout. But what happens when the medicine that’s supposed to help starts making you feel worse? Side effects are more common than most people think, and knowing which ones are normal versus dangerous can make all the difference.
What Counts as a Side Effect?
A side effect, or adverse drug reaction (ADR), is any unwanted reaction to a medicine at a normal dose. It’s not a mistake. It’s not always your fault. Even safe, FDA-approved drugs can cause side effects because the human body is complex. A drug meant to calm your nerves might also make you dizzy. One that reduces stomach acid might leave you constipated. These aren’t rare oddities - they’re built into how the drug works. There are two main types of side effects. Type A reactions are predictable. They’re tied to the drug’s main action. For example, blood pressure meds like metoprolol often cause drowsiness or lightheadedness because they slow down your heart rate. These make up 75-80% of all side effects. Type B reactions are trickier. They’re rare, unpredictable, and not related to the drug’s intended effect. Think allergic rashes, liver damage, or severe skin reactions. These are harder to spot before they happen, but they’re the ones that need immediate attention.Most Common Side Effects You’ll Actually Experience
You don’t need to panic over every little change. Many side effects are mild and go away after a few days as your body adjusts. The most frequent ones across almost all medications include:- Nausea or upset stomach
- Constipation or diarrhea
- Dry mouth
- Drowsiness or fatigue
- Headache
- Mild rash or itching
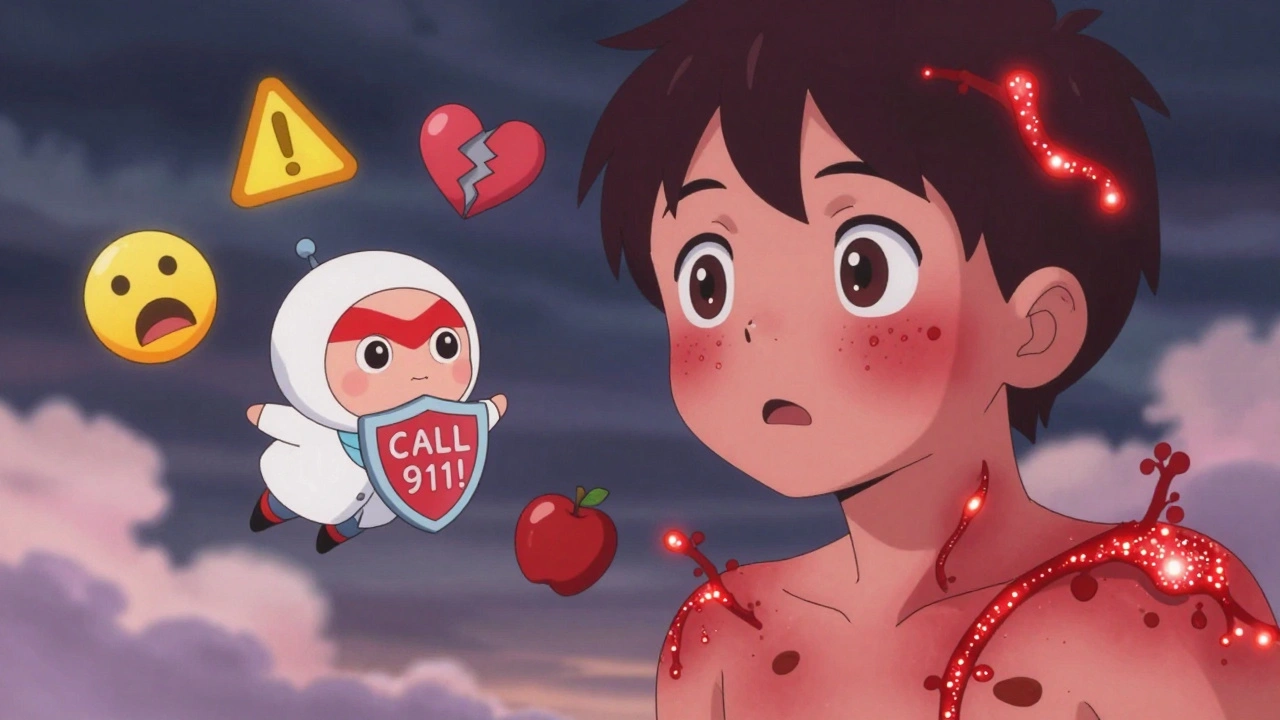
When Side Effects Turn Dangerous
Not all side effects are harmless. Some are medical emergencies. The FDA defines a serious side effect as one that leads to death, hospitalization, permanent damage, or birth defects. Here are the red flags you should never ignore:- Difficulty breathing, swelling of the face, lips, or throat - This could be anaphylaxis, a life-threatening allergic reaction.
- Severe skin rash with blistering or peeling - This might be Stevens-Johnson Syndrome or toxic epidermal necrolysis, rare but deadly skin conditions.
- High fever, swollen lymph nodes, yellowing skin or eyes - These could signal DRESS syndrome, a systemic reaction that damages organs like the liver or kidneys.
- Unexplained bruising, bleeding, or dark stools - Could mean internal bleeding from blood thinners or NSAIDs.
- Fast, irregular heartbeat or fainting - Some antibiotics, antidepressants, and even antihistamines can mess with heart rhythm.
- Sudden confusion, memory loss, or hallucinations - Especially in people over 65, this could be delirium from benzodiazepines or anticholinergics.
Why Older Adults Are at Higher Risk
People over 65 are nearly three times more likely to be hospitalized because of side effects than younger adults. Why? Three big reasons:- Multiple medications - Many seniors take five or more pills a day. Each one adds a new chance for interaction.
- Slower metabolism - As we age, our liver and kidneys don’t clear drugs as quickly. That means drugs stick around longer, increasing the chance of buildup and toxicity.
- Underlying conditions - Diabetes, heart disease, or kidney problems can make side effects worse.

Drug Interactions: The Hidden Danger
Side effects don’t always come from one drug alone. They often come from combinations. Grapefruit juice is a classic example. It can make blood pressure and cholesterol drugs like atorvastatin or felodipine too strong, leading to dangerous drops in blood pressure or muscle damage. Alcohol is another silent killer when mixed with opioids, sedatives, or even some antibiotics. One study found that nearly half of people stop taking their meds within a year - and nearly 30% of those cases were because of side effects made worse by interactions. Even supplements can cause trouble. St. John’s Wort, often used for mild depression, can interfere with birth control, antidepressants, and blood thinners. Garlic pills can thin your blood too much if you’re already on warfarin. Always tell your doctor or pharmacist about every pill, herb, or vitamin you take - even if you think it’s harmless.Chemo and Radiation: The Heavy Hitters
Cancer treatments are different. They’re designed to kill fast-growing cells - but they can’t tell the difference between cancer cells and healthy ones like hair follicles, bone marrow, or gut lining. That’s why side effects are so intense:- Hair loss - usually temporary, but emotionally devastating
- Extreme fatigue - often worse than regular tiredness
- Nausea and vomiting - still common, but better controlled now with modern anti-nausea drugs
- Low blood counts - leading to infection risk, bruising, or shortness of breath
- Diarrhea or constipation - depending on the area being treated
- Loss of appetite or trouble swallowing - especially with head or neck radiation
- Infertility or early menopause - if treatment targets the pelvic area
When to Call Your Doctor - And When to Go to the ER
You don’t need to panic over every sneeze. But you should act fast if:- A side effect is new, worsening, or doesn’t go away after a week.
- You’re having trouble breathing, swallowing, or speaking.
- Your skin is peeling, blistering, or turning red.
- You feel confused, disoriented, or have sudden memory loss.
- You notice unexplained bruising, bleeding, or dark urine.
- You have chest pain, palpitations, or fainting.
How to Report Side Effects - And Why It Matters
You might think reporting a side effect won’t make a difference. But it does. In the U.S., the FDA’s MedWatch program collects over 1.8 million reports each year. Most come from doctors, but patients can report too. The same goes for the Yellow Card Scheme in the UK or EudraVigilance in Europe. Why report? Because side effects that happen to one person might happen to thousands. A rare skin reaction reported by one patient led to the withdrawal of a psoriasis drug called Raptiva after it caused fatal brain infections. If no one had spoken up, more people would’ve been harmed. Even if you’re not sure if it’s related to the drug - report it anyway. Regulatory agencies look for patterns. One report might be noise. Ten reports from different people? That’s a signal.What You Can Do Right Now
You don’t have to wait for a crisis to protect yourself. Here’s what works:- Read the leaflet - Every prescription comes with a patient information sheet. It lists common and serious side effects.
- Use trusted databases - The National Library of Medicine’s Drug Information Portal is free and reliable.
- Keep a side effect journal - Note when symptoms start, how bad they are, and what you were taking. Bring it to appointments.
- Ask questions - “What are the most common side effects?” “Which ones mean I should call you?” “Is this drug safe with my other meds?”
- Don’t stop cold turkey - Some meds, like antidepressants or blood pressure pills, can cause dangerous withdrawal symptoms if stopped suddenly. Talk to your doctor first.



Comments
Ugh, I took that blood pressure med last year and felt like a zombie for 3 weeks. Just quit. My doctor was like 'it's normal' but bro, if normal means I can't walk to the fridge without falling, then no thanks. 😴
I appreciate how you broke this down. I’ve been on statins for five years now and only recently realized my chronic fatigue wasn’t just aging-it was the drug. I started keeping a journal like you suggested, and it actually helped me spot patterns. Now I talk to my pharmacist before picking up anything new. It’s scary how little people are told about what’s in these pills. We’re just expected to take them and shut up.
people these days think every little tummy ache is a side effect. i took ibuprofen once and got a headache. that doesnt mean its dangerous. you just gotta be tough. stop being so sensitive. its not the drugs, its you.
Benadryl = zombie mode. Done.
I just want to say how important it is that you included the part about older adults. My mom was on three different meds that all interacted, and no one ever sat down with her to explain it. She ended up in the hospital after a fall-turns out it was the antihistamine she’d been taking for ‘a little allergy’ for ten years. She’s okay now, but I wish someone had warned us earlier. Please, if you’re caring for someone older, don’t assume they know what’s in their pills. Sit with them. Read the leaflet together. It’s not a chore-it’s love.
The real tragedy here isn’t the side effects-it’s the institutionalized pharmaceutical nihilism that normalizes them. We’ve commodified bodily autonomy under the guise of ‘efficiency’ and ‘evidence-based practice.’ The FDA’s MedWatch program? A performative gesture. A placebo for accountability. Meanwhile, the real villains-pharma’s marketing arms, the ghostwritten clinical trials, the ghosted patient voices-are still cashing checks. We’re not patients. We’re data points with pulse rates.
Fascinating how the pharmacokinetics of aging intersect with polypharmacy in geriatric populations-especially when considering CYP450 enzyme downregulation. 🤔 But let’s not ignore the psychosocial dimension: the normalization of side effects as ‘just part of growing old’ is a neoliberal myth. We’ve outsourced bodily sovereignty to Big Pharma’s algorithmic consent forms. Also, grapefruit juice is a metabolic saboteur. 🍊💥
I’ve been researching this a lot since my dad had a DRESS reaction to allopurinol. What’s wild is how underreported these cases are-most patients don’t know they can report, and doctors often don’t ask. I built a simple web tool to help people log symptoms and auto-generate MedWatch reports. If anyone wants access, DM me. We need more grassroots data collection. Science doesn’t happen in labs-it happens in living rooms, kitchens, ER waiting rooms.
I CAN’T BELIEVE PEOPLE STILL TAKE BENADRYL FOR SLEEP!! IT’S LIKE DRINKING POISON AND CALLING IT A NIGHTCAP!! MY COUSIN HAD A SEIZURE FROM IT!! WHY IS THIS STILL ON THE SHELF?!?!?!?!!!
Y’all in the US are so soft. In my country, we just take the medicine and deal. If you feel weird, you’re weak. America: where a headache is a crisis and a pill is a conspiracy. We don’t need your journals, your apps, your ‘side effect tracking.’ Just shut up and swallow.